Mast cells are made in our bone marrow and travel to various areas of the body where they live for 2-4 years and serve as a sentinel to protect against assaults that might cause harm to the body. They concentrate in the areas of the body where there is an interface between the body and the external environment such as the mucosal surfaces of the gastrointestinal tract, the genitourinary tract, the respiratory tract, and they are also in the connective tissue and the skin. Unfortunately, Mast cells’ efforts to protect us is a reason why we feel allergic and experience inflammation when they are activated.
Mast cells contain granules that secrete multiple chemicals such as:
neurotransmitters histamine, and serotonin
Serine proteases such as tryptase, and chymase
Proteoglycans such as heparin (an anticoagulant)
Lysosomal enzymes such as B-hexsamineidase, B-glucuronidase, and arylsulfatases Cytokines such as TNF alpha, interleukin four, stem cell factor, chemokines, and eosinophil chemotactic factor
Lipid mediators (eicosanoids) such as thromboxane, prostaglandin D2, leukotriene C4, platelet activating factor.
Mast cells can also attack bacteria, viruses, and parasites. Mast cells are also involved with angiogenesis which is the growth of new blood vessels. To do this it secretes VEGF, bFGF, TGF-beta, TGF-alpha, and IL-8.
The degranulation process that occurs from mast cells is not likely to cause problems with most people. When problems arise, it is because it happens more often with less stimulation than is typical. If too many mast cells are degranulating then the body will suffer more from this natural reaction than it would from the threat itself. Systemic mastocytosis is a serious but rare condition which has genetic connections. Cutaneous mastocytosis, also known as Urticaria pigmentosa, is an unsightly skin condition more common in infants but it can affect adults and can be associated with other symptoms such as flushing, heart palpitations, anaphylactic shock, and faintness.
It is mast cell activation syndrome (MCAS), which is the most common manifestation of this overreaction by the mast cell seen today. This could have genetic predisposed triggers or acquired triggers which could be a result of a chronic bacterial infection or a toxin within the body. It could be triggered by hormonal changes, temperature changes, foods, or fragrances. In 1991 a study from Vanderbilt University published a study proposing this new idea and in 2007 the first case reports of what is now called Mast Cell Activation Syndrome were published. It is estimated that anywhere from 1-17% of all people could be suffering from MCAS. Cases of asthma, migraines, hives, itchy skin, Crohn’s disease, GERD, IBS, Lyme, diabetes, Sjogren’s disease, endometriosis, premenstrual syndrome, fibromyalgia, neuropathic pain, chronic sinusitis, prostatitis, chronic urinary infections, and brain fog could all be associated with this phenomenon involving mast cells and this association could be easily missed by most doctors.
Determining whether someone has MCAS is tricky. Science says that testing for histamine or tryptase elevations in the blood is an effective way of determining MCAS but oftentimes those levels are normal when testing unless the patient is having an active reaction at the time of the blood draw. There is research showing urine tests to confirm the MCAS diagnosis that I hope to find out more about to order and these two organizations offer information beyond this newsletter. https://tmsforacure.org/ and https://www.mastcellaction.org/
Medications can be used to tell what kind of granulocyte chemical is being released. If an antihistamine that blocks the H1 receptor such as Zyrtec, Allegra, or Benedril helps or if a H2 receptor agonist for stomach acid such as Pepcid or Zantac helps then it could be a histamine problem, if a NSAID such as aspirin or ibuprofen helps then it is a prostaglandin trigger, if Singulair helps then it is probably a leukotriene problem. Lastly if antibiotics give relief, then there is a chronic bacterial infection. Sodium chromolyn is a medication that is used to stop allergic reactions for mastocytosis. It is a purified flavonoid that stops the degranulation process. This is called a mast cell stabilizer. For some people with MCAS, carrying an epi pen is recommended.
Natural Treatments
Using medications as the mechanism of how to approach MCAS gives us an avenue in determining what natural products might be useful. To modulate histamine, Curcumin, Vitamin D3 and K2, flavonoids such as Quercetin, zinc, and the medication LDN (low dose naltrexone is useful).
If you have trouble metabolizing the breakdown of histamine, there are three pathways that do so and each of them have their own associated nutrients needed to activate the pathway. The first pathway is N.A.T. or N acetyl transferase pathway which needs vitamin B5 or pantethine for it to function properly. The second pathway is the histamine N methyl transferase (HNMT) pathway which means you cannot break down the histamine by methylation and this is an indication you need methyl donors such as methyl folate. Some people have a genetic weakness in this area. The third pathway where histamine is broken down, is the DAO pathway which stands for diamine oxidase pathway. This pathway needs diosmin, vitamin C, vitamin B6 which is P-5-P or pyridoxal five phosphate, magnesium, and copper.
To help reduce a leukotriene trigger, the following should be considered: Boswellia, Luteolin, Apigenin, EGCG (epigallocatechin-3-gallate) found in green tea, Ginger, Milk Thistle, Resveratrol, and Omega 3 fats.
Final Thoughts
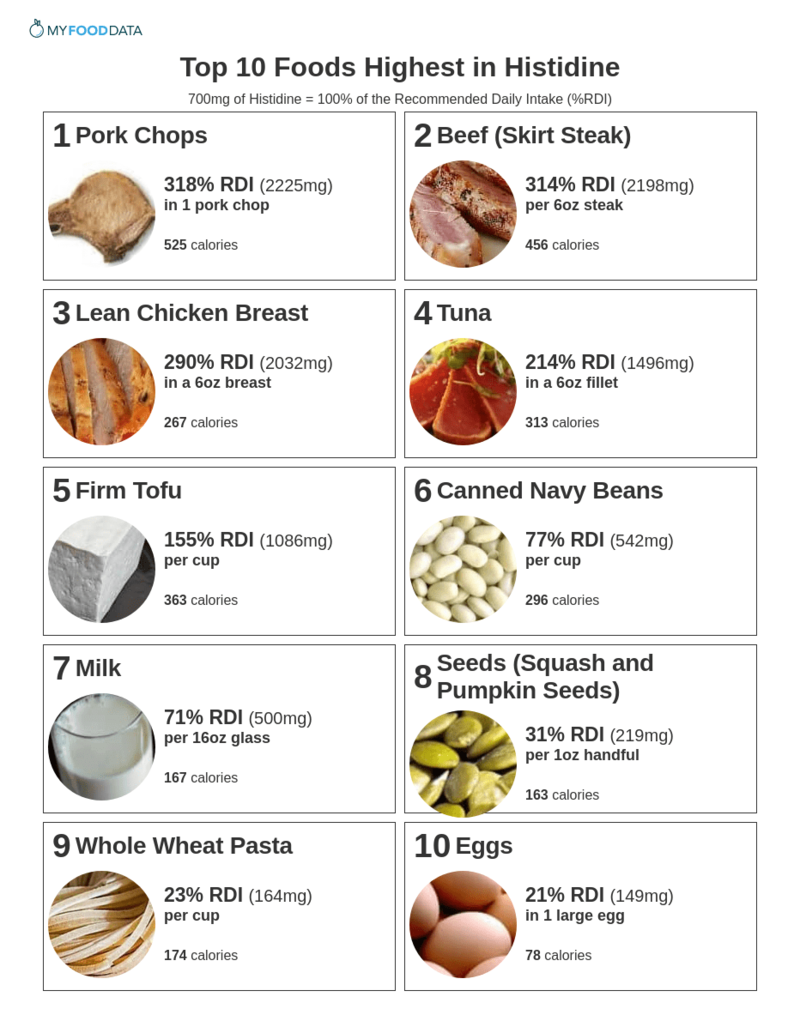
An amino acid histidine (notice the d instead of the m) is plentiful in foods and can be converted into histamine. Some foods have histamine in them. If you have symptoms described with MCAS it would be useful to reduce exposure to those foods. Here are two charts: One is foods with the highest amount of histidine and the other is a chart with the highest amount of histamine, foods that cause the release of histamine and those that block the DAO pathway. The charts do not include leftovers which are another exposure to histamine.