Fibromyalgia Syndrome
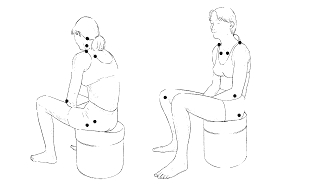
Fibromyalgia was a condition first noticed and described in the early 1900’s by Sir William Gowers. Over the next seven decades more physicians were noticing similar findings and in 1987 a diagnostic code for Fibromyalgia Syndrome (FMS) was instituted along with a consensus of diagnostic criteria to meet that diagnosis. The consensus was that 11 out of an agreed upon 18 diagnostic points would be tender to less than approximately 2 lbs. of finger pressure. These bilateral points were the inner knee, hips, gluteus muscles, trapezius muscles, lower cervical vertebra, lateral epicondyle, second rib anteriorly, occiput bone, and supraspinatus muscles.
In 1992, The Copenhagen Declaration added that FMS was a painful, non-articular condition. It is often associated with persistent fatigue, non-refreshing sleep and that women were 10-20 times more likely to suffer from it than men. It was also associated with headaches, irritable bowel syndrome, cold sensitivity, patterns of numbness and tingling, exercise intolerance and complaints of weakness. Depression and anxiety are also associated with the diagnosis.
Dr. David Brady has separates what he terms “Classic Fibromyalgia Syndrome (CFMS)” from “Pseudo Fibromyalgia (PFMS)” in his forthcoming book The Fibro Fix. In his book he describes the great mimickers of Fibromyalgia. These are described below.
Classic FMS (CFMS) Pseudo FMS (PFMS)
Sleep disorders 1. Organic diseases
Anxiety syndrome 2. Functional disorders
Depression 3. Musculoskeletal disorders
Alterations of brain chemistry
Brain injury/trauma Organic diseases
Anemia, Lyme disease, hypothyroidism, M.S., Cancer
Functional disorders
Poor diet, Nutritional deficiencies, IBS, Gut Dysbiosis, Impaired liver detox pathways, Adrenal dysfunctions,
Medication side effects, Mitochondrial dysfunctions
Musculoskeletal disorders
Posture distortions, muscle imbalance, disc lesions
In classic fibromyalgia there does seem to be a strong family history of emotional trauma or abuse resulting in low serotonin or other neurotransmitters. Patients display behavior of hypervigilance where they are in a constant state of stress and worry about personal safety. In these circumstances there has been some benefit to short term medical intervention with anti-depressants, both SSRI’s and SSNRI’s, but both have serious side effects to be wary of. In CFMS, the pain isn’t in the muscle itself, but is perceived pain in the brain. In CFMS, pain throughout the body is being amplified by the central nervous system. Neurologically this has been linked to the Descending Antinociceptive System (DANS) in the spinal cord. It is here where something called Substance P is elevated in CFMS patients. Substance P lowers pain thresholds and activates larger receptive fields which “spreads the pain”. There have been studies that have shown an inverse level of serotonin and substance P, along with a low T3 thyroid hormone and Substance P. So with low serotonin and low T3 there is high Substance P!
Some examples of PFMS are Hashimoto’s hypothyroid, mitochondrial dysfunction, and gut dysbiosis. Hashimoto’s Thyroid is an autoimmune thyroid meaning that the body’s immune system is attacking their own thyroid and this results in lowered amounts of the active thyroid hormone, T3. Auto immune conditions are common with food sensitivities. In mitochondrial dysfunction, the likely cause comes from the ubiquitous exposure of chemicals, and pesticides, etc. in our environment. Statins for lowering cholesterol are mitochondrial toxins. To improve mitochondrial function, vitamins such as those in the B complex family, Coenzyme Q10 and amino acids such as L-Carnitine, Arginine, Glycine, Citrulline, and Glutathione have shown to be helpful. Gut dysbiois is a condition where the normal internal microflora of the intestinal tract has been infiltrated by abnormal microbes such as yeast, bacteria, virus’ or parasites. This can cause an inflammatory reaction to the enteric nervous system and central nervous system. In fact, Dr. Brady feels that Irritable Bowel Syndrome is really CFMS of the gut. The enteric nervous system of the gastrointestinal system has pain fibers that amplify pain just like the brain does and those pain signals are dampened with the normalization of serotonin levels just like it is in peripheral muscles.
Conclusion
Before 1984 the number of research articles on Fibromyalgia ranged from 10-30 per year. Now the number is between 100-140 per year. The increase in research is correlating with an increasing number of these patients appearing in physician’s offices. The challenge for clinicians, is to do a careful history to determine if the symptoms of Fibromyalgia are from organic, functional or structural causes. The over prescribing of anti-depression medication, sleep medications, and especially opioid pain medications has led in some cases to serious drug dependencies. There are natural approaches to increase serotonin that need to be given more consideration such as 5HTP and probiotics. Dietary changes and using botanicals like Valerian to calm the nervous system or Turmeric to help with pain are the kind of natural compounds that will be used more widely for those suffering with this disorder in the future.